Centers for Medicare & Medicaid Services (CMS) is preparing to launch the Transforming Episode Accountability Model (TEAM) on January 1st, 2026. While CMS has experimented with value-based incentives for hospitals before – notably Bundled Payments for Care Improvement Advanced (BPCI-A) – TEAM marks a new chapter. With mandatory participation, regional benchmarks, and compressed timelines, TEAM presents both risks and opportunities for hospitals.
From BPCI-A to TEAM:
What Hospitals Need to Know
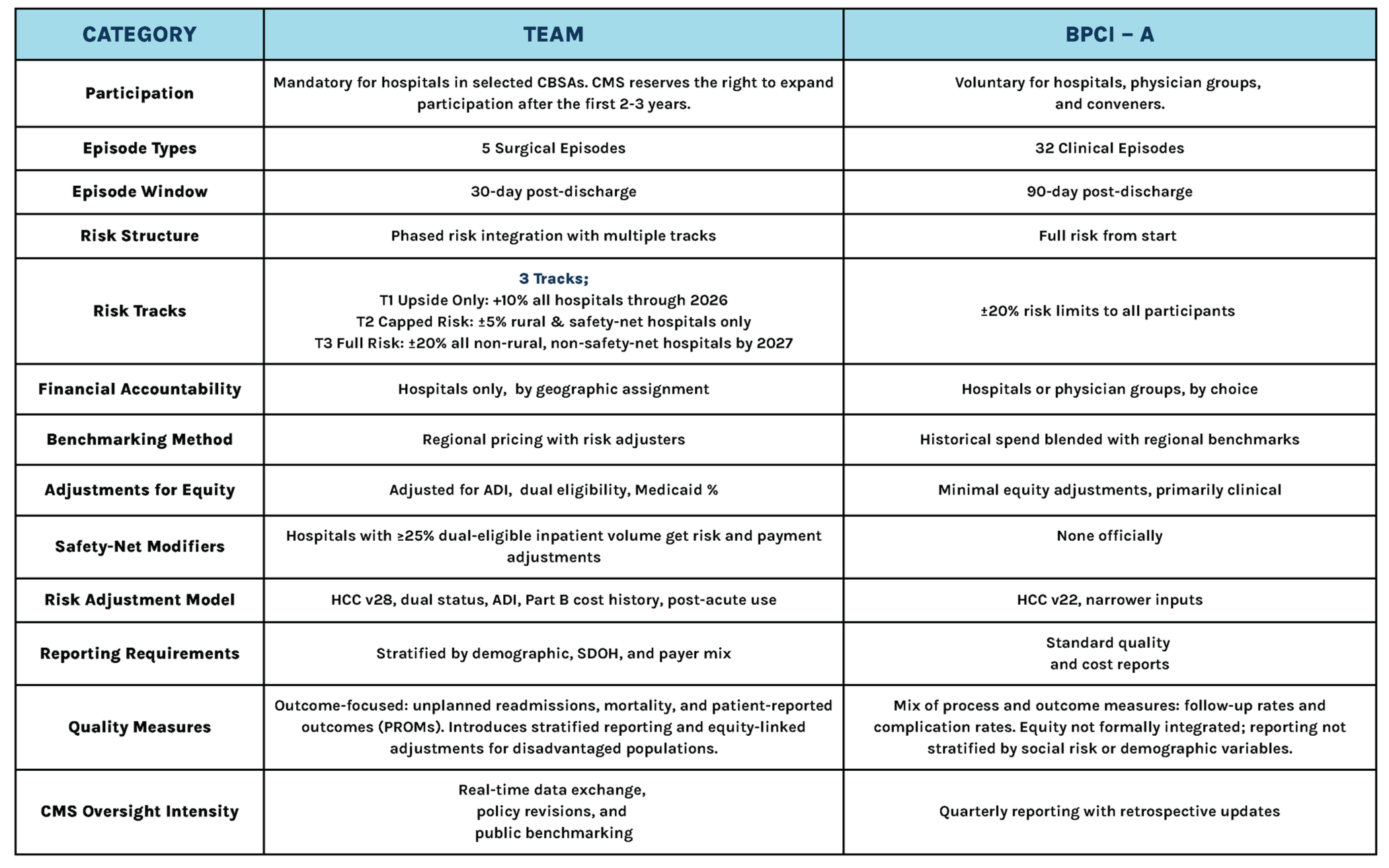
Comparing TEAM & BPCI – A
Benchmarking is a key point to prepare for in TEAM, as hospitals will now be compared to their peers. This puts increased emphasis on upstream risk adjustment, meaning hospitals must begin documenting SDOH and clinical complexity well before hospitalization. In most cases, risk scores must be captured 6 months before the episode begins to ensure appropriate benchmarks and equity modifiers.
Increased diagnosis requirements are compounded by TEAM shortening the accountability duration from 90 to 30 days. The shorter window reduces the ability to smooth out costs. In BPCI-A, a patient who is readmitted early could be mitigated through lower home health, rehab, or other spending. A single readmission or unnecessary SNF day could take a patient over the allotment, passing on costs to hospitals. The first 72 hours post-discharge are key, placing more pressure on discharge planning and care transitions.
TEAM is intended to narrow the focus and accountability from the BPCI – A framework, and reflects a commitment to value-based care.
TEAM’s elimination of conveners from the model is one of the most consequential and overlooked aspects. In BPCI-A, conveners played a central role: aggregating providers, managing data, coordinating care redesign, and often assuming financial risk on behalf of hospitals or physician groups. For many hospitals, particularly smaller and those with less infrastructure, conveners were the engine that made BPCI-A feasible. TEAM removes this buffer. Participants must now contract directly with CMS, bear their own financial risk, and independently manage care coordination, analytics, and reporting. The removal of third-party delegation signals that the future of value-based care rests on provider accountability. Hospitals that thrived under BPCI–A with the help of conveners must now rapidly stand up internal capabilities and partner differently to succeed in TEAM.
Your Health specializes in at-home senior care, providing primary care, physical therapy, and more for our patients. We are already committed to value-based care and emphasize frequent visits by a multidisciplinary team to keep our patients out of the hospital. In preparation for TEAM, we are building dedicated care groups to partner with hospitals in CBSAs.
To explore how Your Health can support your TEAM readiness, contact us here: